10 Important FQHC Billing Tips to Boost Revenue
Posted by Jane Kirsty Pardo
Healthcare Technology FQHC Community Health
The healthcare reimbursement system is complicated. It's a frustrating fact that providers often have no choice but to accept. This has led insurance companies, practices, and even patients to become vigilant with their money. The same is true even for Federally Qualified Health Centers (FQHCs), where providers continue to face billing and reimbursement challenges, not to mention the complex and confusing rules and processes set by insurance companies.
As the demand for public health facilities increases, providers are now under increased pressure to receive higher reimbursements and cut operating costs. However, denials, underpayments, and lost or ignored claims keep weighing practices down.
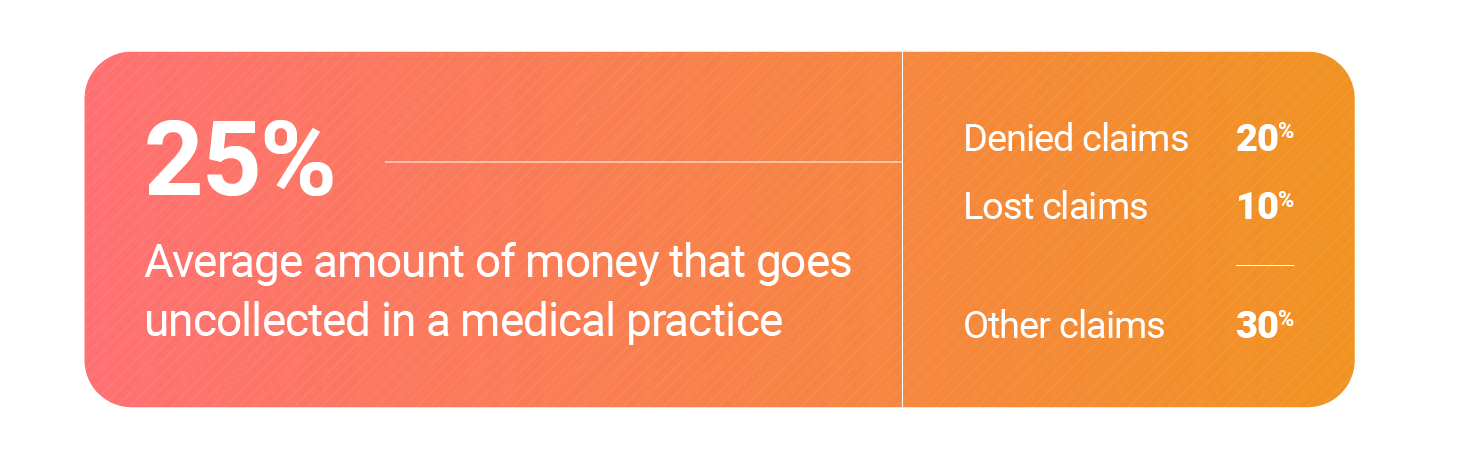
Source: Center for Medicare and Medicaid Services (CMS)
How can your clinic reclaim those missing funds? The best way to do so is to improve the overall efficiency of your billing and collections, but that’s just another challenge altogether. To help you tackle this particular challenge, here are 10 important FQHC billing tips:
1. Enable more ways to get paid. Make sure that you maximize the use of all channels where your patients can make payments.
2. Make payments more convenient. Allow your patients to quickly pay bills online or through any mobile device.
3. Streamline the gathering of billing information. Eliminate redundant forms and always aim for accuracy when capturing your patient’s billing information.
4. Make payments more secure. Security is the number one concern of your patients. Make sure that they can maintain their peace of mind when they make payments.
5. Improve your billing workflow. Less work means less room for errors. To avoid inefficiencies, choose an EHR that matches your billing workflow.
6. Verify patient insurance eligibility in advance or in real-time. If you miss this step, this might be the reason for denials or lost claims.
7. Observe an efficient claims management process. Save your staff from the time-consuming task of checking for claims and going back and forth. Make sure to catch claims errors before they’re made.
8. Eliminate claims errors. Choose an EHR with a comprehensive list of CPTs and HCPCS that will allow you to document without the hassle.
9. Choose an EHR with efficient reporting capabilities. Auditing payments can be tricky. Make it easier for your staff to audit payments received against all payer contracts and make sure that you’re paid accordingly.
10. Choose an EHR with a built-in billing platform. There shouldn’t be any third-party software and unnecessary fees that may mean more expenses than revenues.
Managing your billing processes can be tough. One major step towards a more efficient billing and collections workflow is to select a software solution that’s specifically designed for your health center. Putting in place a comprehensive, accurate, and (most of all) automated billing and collections workflow not only saves your clinic time and money, but it also allows you to focus more on what you do best—caring for your patients.
.png?width=598&name=%5BBLOG%5D%2010%20Important%20FQHC%20Billing%20Tips%20to%20Boost%20Revenue_Image%203%20(1).png)
Share this post: on Twitter on Facebook on Google+


